Inside This Issue: Report Examines on Social Determinants of Health and HIV, Role of Self-Testing in Ending the HIV Epidemic, FDA Permits Marketing of First Condom Specifically for Anal Intercourse, Impact of the Ukraine War on HIV Services, New Community-Level Approach for Classifying COVID-19 Risks, and more

Social Determinants of Health
CDC Surveillance Report Examines Social Determinants of Health and HIV
Social determinants of health (SDH) have a strong correlation with the HIV care continuum among U.S. adults with HIV, according to a new CDC HIV surveillance report. SDH refers to the nonmedical factors that influence health outcomes. “They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life,” according to CDC. “These forces and systems include economic policies and systems, development agendas, social norms, social policies, and political systems that are responsible for most health inequities, including the disproportionate effect of HIV on certain populations.”
To examine the interrelationship of SDH and HIV, researchers correlated HIV surveillance data with census tract data for several SDH indicators, including:
- Federal poverty status, defined as the percentage of persons in the census tract living below the federal poverty level;
- Median household income in the census tract;
- Education level, defined as the percentage of the adult population in the census tract with less than a high school education;
- Health insurance coverage rates in the census tract; and
- The Gini index, a measure of income inequality.
For their analysis, the CDC researchers divided each of the SDH indicators for census tracts into four tiers, corresponding to lowest to highest levels of poverty, household income, and so forth. In addition to analyzing these SDH indicators for all adults in census tracts, the researchers also broke down the SDH data by sex at birth, age, race/ethnicity, and transmission category.
Their analysis for 2019 revealed that rates of HIV diagnosis, prompt linkage to HIV care, and HIV viral suppression were strongly correlated with the five SDH indicators. The report includes a Special Focus Profiles section that “highlights disparities in rates of HIV diagnoses by SDH variables, including income inequality, and factors for special consideration in addressing health disparities that may be of particular interest to HIV prevention programs in state and local health departments.” It includes analyses of relative and absolute disparities in HIV diagnoses by race/ethnicity for the SDH variables, summarized both in text and infographics:
- Federal poverty level status, for adult males and adult females;
- Education status, for adult males and adult females;
- Income level, for adult males and adult females;
- Health insurance coverage rates, for adult males and adult females; and
- Income inequality, for adult males and adult females
The final part of the Special Focus Profiles examines three important factors that merit special consideration when addressing and reducing SDH-related health disparities among adults with diagnosed HIV infection – residential racial segregation, medical treatment, and psychosocial stress.
HIV Testing and Prevention
The Role of Self-Testing in Ending the U.S. HIV Epidemic
CDC recently published an issue brief that considers the role that HIV self-testing may play in U.S. efforts to end the HIV epidemic. “In 2020, HIV testing decreased noticeably across the country as the COVID-19 pandemic made it more difficult to access traditional, in-person testing services,” CDC notes. “HIV self-testing programs offer an innovative way to bridge gaps in access to HIV testing and ensure that HIV testing is simple and more accessible for all.” The brief provides detailed information about the benefits of HIV self-testing; the agency’s current efforts to make HIV self-testing simple, accessible, and routine; and the steps different stakeholders – including federal health agencies, state and local health departments, community-based organizations (CBOs), healthcare providers, and elected and community leaders – can take to sustain and build on recent progress in HIV self-testing. CDC also spotlights three recent health department and CBO programs to promote and support self-testing. For additional information on this topic, you can visit NEAETC’s Online HIV Resource Library page focusing on HIV Testing.
FDA Permits Marketing of First Condom Specifically for Anal Intercourse
Late last month, the U.S. Food and Drug Administration (FDA) authorized the marketing of the first condoms specifically indicated to help reduce transmission of HIV and other sexually transmitted infections (STIs) during anal intercourse. FDA has also authorized the product, marketed as the One Male Condom, to help prevent STI transmission during vaginal intercourse and as a contraceptive to reduce the risk of pregnancy. The agency noted that, while the recent authorization underscores the public health importance of condoms tested and labeled specifically for anal intercourse, all other FDA-cleared condoms can continue to be used for contraception and STI prevention.
“The risk of STI transmission during anal intercourse is significantly higher than during vaginal intercourse,” noted Dr. Courtney Lias of FDA’s Center for Devices and Radiological Health. “The FDA’s authorization of a condom that is specifically indicated, evaluated, and labeled for anal intercourse may improve the likelihood of condom use during anal intercourse. Furthermore, this authorization helps us accomplish our priority to advance health equity through the development of safe and effective products that meet the needs of diverse populations.”
U.S. HIV Workforce
Survey Study: National Evaluation of HIV Primary Care Workforce
The AIDS Education and Training Center Program National Coordinating Resource Center (NCRC) is conducting a National HIV Workplace Study to evaluate the number of currently practicing U.S. healthcare providers prescribing HIV antiretroviral treatment (ART), as well as the number of care providers projected to continue to provide HIV-related care in the U.S. over the next 5 years. To participate in the study, one must be a prescribing clinician (either a physician, nurse practitioner, nurse midwife, physician assistant, or pharmacist) who currently provides HIV-related medical care in the U.S., including prescribing ART. Participants agree to complete an online survey that has about 30 questions and takes about 10 minutes, according to NCRC.
Through the survey, researchers hope to learn about:
- the number of clinicians currently providing HIV-related medical care, as well as their demographic and professional characteristics;
- the current market demand and need for HIV-related medical services in the U.S., and how this varies by geographical region;
- the factors that will influence the future supply of U.S.-based HIV clinicians and the future demand and need for HIV-related medical services; and
- whether the projected supply of HIV-related clinicians in the future will be sufficient to meet the demand and need for HIV-related medical care in the U.S., including in different geographic regions.
The Global HIV/AIDS Epidemic
UNAIDS: Perspectives on the Impact of the Ukraine War on HIV Services
In the wake of Russia’s invasion of Ukraine, UNAIDS has published a series of features that provide news and perspectives on the impact of the war on HIV services in Ukraine and Eastern Europe. One article describes the efforts of the All-Ukrainian Association of People with Drug Addiction, which is continuing, despite the war, to provide harm reduction services, food, and water to people who inject drugs in Ukraine. A second article describes the work of 100% Life, the largest network serving people with HIV in Ukraine, to evacuate, relocate, and keep people with HIV safe, and to maintain their access to antiretroviral treatment as the war continues.
And in an opinion piece, Michel Kazatchkine, special advisor to UNAIDS on HIV/AIDS in Eastern Europe and Central Asia, makes the case that facilities in Ukraine and Eastern Europe “must be protected, be functional, safe, and accessible to all who need essential medical services, and health workers must be protected.” The region, which includes Russia, is the home to about 1.6 million people with HIV. There are nearly 150,000 HIV infections each year, with drug use accounting for about half that total. Unlike Russia, which opposed opioid agonist therapy (OAT) for people who inject drugs, Ukraine “is a notable champion of harm reduction, including OAT and needle exchange programs. This matters greatly in Eastern Europe and Central Asia which continues to be home to the fastest growing HIV epidemic in the world,” according to Kazatchkine.

Conference Reports
More News from CROI 2022
Since the publication of this month’s In Brief issue devoted to the 2022 Conference on Retroviruses and Opportunistic Infections (CROI 2022), several sites have provided summaries of important news from the conference. These include:
- HIV research update from CROI 2022 with NIH’s Dr. Carl Dieffenbach: Cancer prevention, aging, and the future of HIV prevention & treatment (HIV.gov)
- A Round up from CROI 2022 (AVAC)
- Top 5 HIV cure and vaccine stories from CROI 2022 (AIDSmap)
- Top 5 HIV treatment stories from CROI 2022 (AIDSmap)
- Top 5 stories on HIV prevention from CROI 2022 (AIDSmap)
- Top 5 stories on HIV, ageing, and co-morbidities from CROI 2022 (AIDSmap)
- Top 5 stories on HIV treatment and care in Africa from CROI 2022 (AIDSmap)
Other news outlets that have published additional coverage from CROI 2022 during the past few weeks, include: AIDSmap, HIV Treatment Bulletin, NATAP, and Poz.

Educational Resources
Updated CDC Resources on Groups Affected by HIV
In recent weeks, CDC has published online several updated resources that provide an overview of the impact of HIV on people in particular demographic groups and those at high risk for HIV. These recently updated web pages and fact sheets summarize information about new HIV diagnoses, HIV prevalence, the HIV care continuum, and steps CDC is taking to address the impact of HIV on each featured group:
- HIV and Men
- HIV and Women
- HIV and Pregnant Women, Infants, and Children
- HIV and African American People
- HIV American Indian/Alaska Native People
- HIV and Asians
- HIV and Native Hawaiians and Other Pacific Islanders
- HIV and Youth
- HIV and Older Americans
- HIV Risk Among Persons Who Exchange Sex for Money or Nonmonetary Items
- HIV and People Who Inject Drugs
For additional information on the effects of HIV on different population groups, you can visit NEAETC's Online HIV Resource Library.
Blog Posts and Infographics from AIDSVu Highlight HIV Among Women and Girls
To mark National Women and Girls HIV/AIDS Awareness Day (NWGHAAD) on March 10, AIDSVu published blog items highlighting the impacts of HIV on women and girls. Dr. Adaora Adimora, co-director of the University of North Carolina’s Center for AIDS Research, writes about the impacts of HIV on women and minorities and efforts to increase the use of pre-exposure prophylaxis (PrEP). In another blog item, AIDSVu highlights key facts about HIV among women and girls, with an emphasis on racial/ethnic disparities, and includes the following updated infographics:
- Women Accounted for One-Fifth of All New HIV Diagnoses During 2020
- Racial/Ethnic Disparities in New HIV Diagnoses Among Women
- Modes of HIV Transmission Among Women
- Low Rates of HIV PrEP Use Among Women
- High Unmet Need for PrEP in the South Among Women
- States with Highest Rates of Linkage to HIV Care Among Women
- High HIV Mortality Rates Among Black Women
- Racial and Ethnic Differences in Viral Suppression Rates Among Women
- Social Determinants of Health and HIV Among Women
For additional information on this topic, you can visit NEAETC’s Online HIV Resource Library page focusing on Women and HIV.
COVID-19 News
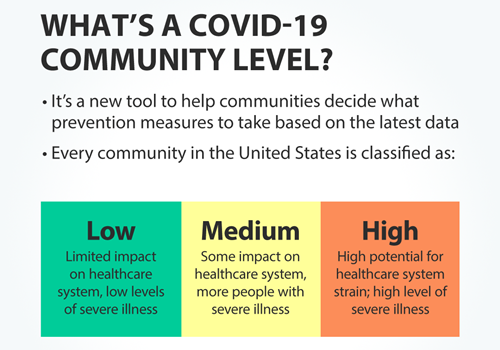
New Community-Level Approach for Classifying COVID-19 Risks
CDC recently adopted a community-level approach for gauging the impact of COVID-19 illness on health and healthcare systems and “to help communities and individuals make decisions based on their local context and their unique needs.” In this approach, CDC uses a combination of three metrics to determine the COVID-19 community level, which is classified as either low, medium, or high. These metrics are: new COVID-19 admissions per 100,000 population in the past 7 days, the percent of staffed inpatient beds occupied by COVID-19 patients, and total new COVID-19 cases per 100,000 population in the past 7 days.
“New COVID-19 admissions and the percent of staffed inpatient beds occupied represent the current potential for strain on the health system,” according to CDC. “Data on new cases acts as an early warning indicator of potential increases in health system strain in the event of a COVID-19 surge.”
CDC’s COVID-19 Community Levels page describes the approach in detail, including cut-off values for the different metrics when determining if the community level is low, medium, or high. The page also includes a U.S. map, updated weekly, that depicts COVID-19 community levels by county. In addition, the page provides recommendations about individual- and household-level COVID-19 prevention behaviors and community-level prevention strategies for areas with low, medium, or high community levels.
Notably, CDC no longer specifically recommends the wearing of masks for people living in areas with low COVID-19 community levels. However, the agency acknowledges that high-risk congregate settings (such as correctional facilities and homeless shelters) and healthcare settings may wish to adapt more stringent prevention measures than those listed in its general guidance. In addition, CDC also notes that people who are immunocompromised or at high risk for serious disease, as well as those with household members or social contacts at high risk, may wish to take additional COVID-19 precautions. Moreover, “At all levels, people can wear a mask based on personal preference, informed by personal level of risk,” according to CDC. “People with symptoms, a positive test, or exposure to someone with COVID-19 should wear a mask.”
Recent Data Summaries and Research Reports
CDC’s COVID Data Tracker Weekly Review highlights key data from its COVID Data Tracker, narrative interpretations of the data, and visualizations from the week. Themes of recent Weekly Review issues include protecting those at high risk for serious illness, COVID-19 community levels, COVID-19 and youth, and the effectiveness of boosters.
The Morbidity and Mortality Weekly Report (MMWR) is also providing continuing coverage of COVID-19-related research. CDC is archiving its MMWR reports on a page devoted to studies about COVID-19. For your convenience, we have compiled below links to recent MMWR papers organized by topic.
Vaccination Coverage, Safety, and Effectiveness
- COVID-19 Vaccine Provider Access and Vaccination Coverage Among Children Aged 5-11 years – United States, November 2021-January 2022
- Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties – United States, December 14, 2020-January 31, 2022
- Safety Monitoring of COVID-19 Vaccine Booster Doses Among Persons Aged 12-17 Years – United States, December 9, 2021-February 20, 2022
- Effectiveness of COVID-19 Pfizer-BioNTech BNT162b2 mRNA Vaccination in Preventing COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Nonimmunocompromised Children and Adolescents Aged 5-17 Years – VISION Network, 10 States, April 2021-January 2022
- Effectiveness of 2-Dose BNT162b2 (Pfizer BioNTech) mRNA Vaccine in Preventing SARS-CoV-2 Infection Among Children Aged 5-11 Years and Adolescents Aged 12-15 Years – PROTECT Cohort, July 2021-February 2022
Transmission
- SARS-CoV-2 Incidence in K-12 School Districts with Mask-Required Versus Mask-Optional Policies – Arkansas, August-October 2021
- SARS-CoV-2 B.1.1.529 (Omicron) Variant Transmission Within Households – Four U.S. Jurisdictions, November 2021-February 2022
- Antigen Test Positivity After COVID-19 Isolation – Yukon-Kuskokwim Delta Region, Alaska, January-February 2022
- Results from a Test-to-Release from Isolation Strategy Among Fully Vaccinated National Football League Players and Staff Members with COVID-19 – United States, December 14-19, 2021
Outbreaks
- Multistate Outbreak of SARS-CoV-2 B.1.1.529 (Omicron) Variant Infections Among Persons in a Social Network Attending a Convention – New York City, November 18-December 20, 2021
- Investigation of SARS-CoV-2 Transmission Associated With a Large Indoor Convention – New York City, November-December 2021
Health Impacts
- Hospitalization of Infants and Children Aged 0-4 Years with Laboratory-Confirmed COVID-19 – COVID-NET, 14 States, March 2020-February 2022
- Pediatric Emergency Department Visits Before and During the COVID-19 Pandemic – United States, January 2019-January 2022
- Pediatric Emergency Department Visits Associated with Mental Health Conditions Before and During the COVID-19 Pandemic – United States, January 2019-January 2022





%20small.jpg)