Inside This Issue: High transmission rates in HIV clusters; HIV partner services update; core HIV indicators; monkeypox in people with HIV; funding for opioid treatment and prevention; and more.
%20small-horz.jpg)
U.S. HIV/AIDS Epidemic
CDC Finds Very High Transmission Rates in HIV Clusters Involving Gay, Bisexual, and Other MSM
Despite advances in HIV prevention and treatment, the number of HIV diagnoses among gay, bisexual, and other men who have sex with men (MSM) in the U.S. totaled nearly 22,000 during 2020. This figure is equivalent to about 71% of all new HIV infections reported to CDC that year. Detecting and responding to HIV clusters – including among MSM – is a core strategy in U.S. efforts to end the HIV epidemic.
To better understand rapid HIV transmission, CDC researchers characterized large HIV molecular clusters detected using analysis of HIV-1 nucleotide sequence data from the National HIV Surveillance System. They found that HIV clusters occurring primarily among MSM accounted for more 29 of the 38 HIV clusters (76%) first detected during 2018 or 2019 that had grown to include more than 25 persons by December 2021. These clusters primarily among MSM occurred in all U.S. geographic regions, and 97% involved multiple states. The researchers found that the persons in these clusters were heterogeneous in age, gender identity, and race/ethnicity. The clusters also grew rapidly, with median growth rates of nine newly infected persons added per year. The overall transmission rate at cluster detection was 22 transmission events per 100 person-years – a figure more than six times that of previously estimated national HIV transmission rates.
“Leveraging cluster data to rapidly identify and implement interventions when clusters are first detected is essential to stopping transmission. Many MSM face barriers to accessing HIV services because of stigma, homophobia, racism, xenophobia, poverty, and limitations in health insurance,” the CDC researchers noted. “Successful response interventions should aim to eliminate these barriers, quickly close service gaps, and address existing and emerging syndemics affecting MSM, including sexually transmitted infections and monkeypox. When mobilized effectively, strategies that engage communities, improve prevention services, and strengthen linkage to care can address the needs of persons in HIV clusters.”
Summaries of Recent CDC HIV Reports
In the past several weeks, CDC has published two reports focusing on HIV partner services and core indicators of the U.S. HIV epidemic. For your convenience, we are providing brief summaries and links to each report below.
Delivery of HIV Partner Services in the United States and Dependent Areas, 2020 – This report summarizes partner services delivery to the 44,440 index patients who were reported across all U.S. HIV Partner Services programs. The 23,252 patients who were interviewed named a total of 12,830 sex and/or needle-sharing partners. Of the 4,245 partners tested with a documented HIV test result, 28% were newly identified as HIV-positive, and 86% with a known care status were linked to care. Of the 2,336 who were HIV-negative, 1,256 had a reported HIV pre-exposure prophylaxis (PrEP) status and 14% were taking PrEP. Of the 1,020 partners not taking PrEP with a reported referral status, 35% were referred to a provider who can prescribe PrEP.
HIV Surveillance Tables: Core Indicators for Monitoring the Ending the HIV Epidemic Initiative (latest issue) – This issue of CDC’s HIV Surveillance Data Tables presents preliminary data for diagnoses of HIV infection reported to CDC through June 2022 and PrEP data reported through March 2022. A total of 11 data tables are included, focusing on:
- new HIV infections among adults and adolescents aged 13 years or older during the period from January 2021 through June 2022;
- linkage to HIV care within 1 month of diagnosis among adults and adolescents during the period from January 2021 through March 2022; and
- number of persons prescribed PrEP, number of persons with PrEP indications, and PrEP coverage among persons aged 16 years or older during the period from January 2019 through March 2022.
The data tables include breakdowns by gender, age at diagnosis, race/ethnicity, transmission category, and region of residence. Specific data are also provided on new HIV diagnoses, the numbers of persons prescribed PrEP and with PrEP indications, and PrEP coverage in Ending the HIV Epidemic Phase I jurisdictions.
Monkeypox Outbreak
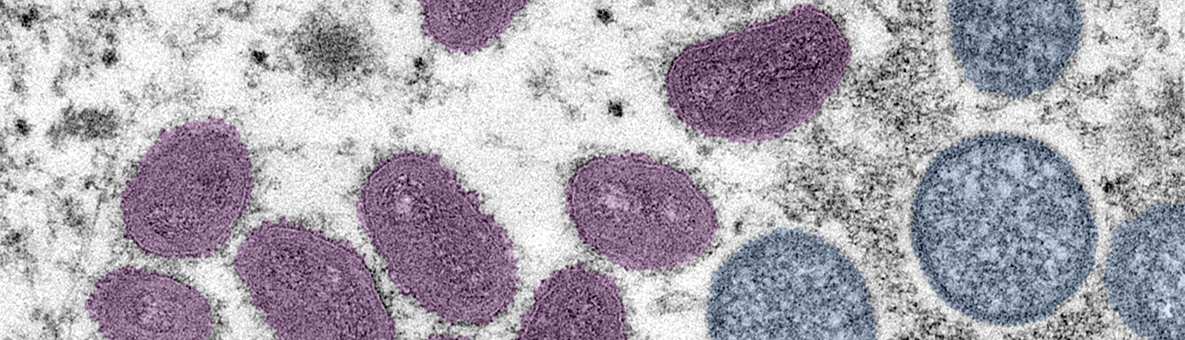
Severe Manifestations of Monkeypox Among People Immunocompromised Due to HIV
On September 29, CDC issued a health advisory to inform health providers that people who are immunocompromised due to HIV or other conditions have a higher risk of experiencing severe manifestations of monkeypox than people who are immunocompetent. CDC noted that, although most people diagnosed with monkeypox have had mild-to-moderate clinical courses, the majority of persons with severe manifestations of monkeypox had HIV with CD4 counts less than 200 cells/ml, indicating substantial immunosuppression. For this reason, CDC is advising providers to determine the HIV status of all sexually active adults and adolescents with suspected or confirmed monkeypox.
During the current outbreak, severe manifestations of monkeypox have included the following:
- atypical or persistent rash with coalescing or necrotic lesions, or both;
- lesions on a significant proportion of the total body surface area;
- lesions in sensitive areas (including mucosal surfaces, such as oropharynx, urethra, rectum, vagina) resulting in severe pain;
- bowel lesions that are exudative or cause significant tissue edema;
- severe lymphadenopathy that can be necrotizing or obstructing;
- lesions leading to stricture and scar formation resulting in significant morbidity; and
- involvement of multiple organ systems and associated comorbidities.
“In immunocompromised people, monkeypox treatment should include optimizing immune function by limiting the use of immunosuppressive medications if not otherwise clinically indicated, and, for those with HIV, providing antiretroviral therapy,” according to CDC. “In addition, there are medical countermeasures that may have a role in treating severe illness, including oral and intravenous tecovirimat (TPOXX), cidofovir or brincidofovir, and vaccinia immune globulin intravenous (VIGIV), although there are no data on effectiveness in treating human monkeypox with these medical countermeasures. Decisions on whether and when to use these medical countermeasures must be made individually for each person and can depend on a variety of clinical and other parameters.”
New Monkeypox Videos and Issue Brief from CDC
CDC has developed a series of brief videos in English and Spanish that provide a variety of information about monkeypox, including the monkeypox virus, transmission, steps to prevent infection, vaccination, testing, and treatment. Although most of the nearly 20 videos currently available address common concerns among persons at risk for monkeypox and the general public, several are specifically for healthcare providers. These include instructions on how to administer the JYNNEOS vaccine intradermally and guidance for providers who suspect that a patient has been exposed to monkeypox.
The agency also recently published an issue brief, Reducing Stigma in Monkeypox Communication and Community Engagement. The brief describes how CDC is framing communication around monkeypox and guidance for messaging around monkeypox, including information for general audiences and gay and bisexual men. Additional guidance is also provided for educational messaging about monkeypox at community events, as well as communication strategies to reduce stigma related to monkeypox.
%20-%20more%20horizontal%20(scrabble%20tiles).jpeg)
U.S. Opioid Epidemic
HRSA Announces Over $100 Million Funding to Expand Substance Use Treatment and Prevention in Rural Areas
Late last month, the Health Resources and Services Administration (HRSA) announced investments totaling more than $104 million to expand treatment and prevention services for substance use in rural areas across the U.S. as part of the Rural Communities Opioid Response Program (RCORP). RCORP is a multi-year initiative whose aim is to reduce the illness and death arising from substance use among rural Americans. Access to substance use treatment is very limited in many rural areas. Nearly 37% of all rural counties – and more than half of all small and remote rural counties – have no clinicians authorized to prescribe the opioid treatment buprenorphine. Rural communities have experienced a consistent rise in drug overdose deaths, with a nearly five-fold increase from 1999 to 2019. Opioid-involved overdose deaths, especially those involving fentanyl, have increased significantly across the U.S. since 2019.
The newly announced awards include the following:
- The Rural Communities Opioid Response Program – Medication Assisted Treatment Access awarded over $10 million to 11 grantees to establish new medication assisted treatment access points for substance use, including opioid use disorder.
- The Rural Communities Opioid Response Program – Implementation awarded $65 million to 65 grantees to strengthen and expand opioid use disorder prevention, treatment, and recovery services in rural communities utilizing workforce development and training, telehealth, health care integration, and family support services.
- The Rural Communities Opioid Response Program – Behavioral Health Care Support awarded $29 million to 58 grantees to improve the quality and sustainability of behavioral health care services in rural communities, including through evidence-based, trauma-informed treatment for substance use.
“Today we are taking action to support the critical needs of rural communities by expanding access to opioid use disorder treatment,” noted HRSA Administrator Carole Johnson. “Too often, the needs and challenges of rural communities are not well understood, but at HRSA, we are focused on reaching the rural communities that need our support the most and helping them tackle the overdose crisis.”
%20small.jpg)
Global HIV/AIDS Response
Global Fund Partners Pledge More Than $14 Billion to Fight AIDS, TB, and Malaria and Prevent Future Pandemics
At the 7th Replenishment Conference for the Global Fund to Fight AIDS, Tuberculosis, and Malaria (Fund) in New York last month, Fund partners pledged a total of more than $14.25 billion to support the Fund’s activities during the next three years. The conference brought together representatives from more than 45 countries, multilateral partners, private sector companies, and civil society and community organizations.
The U.S. has made a commitment to contribute US$6 billion over the next three years – a 30% increase over its previous pledge. Several other long-term public donors also increased their pledges by 30%: Canada pledged CA$1.21 billion; the European Commission pledged €715 million; the Federal Republic of Germany pledged €1.3 billion; and Japan pledged up to US$1.08 billion. The Republic of France also substantially increased its pledge to nearly €1.6 billion. In addition to the approximately $13 billion pledged by individual nations and the European Commission, a total of US$1.23 billion was raised from private sector and non-government donors, led by a pledge of $912 million from the Bill and Melinda Gates Foundation.
Since its inception in 2002, the Fund is estimated to have saved more than 50 million lives and provided prevention, treatment, and care services to hundreds of millions of people. With the newly pledged resources, the Fund aims to save an additional 20 million lives, avert 450 million new infections, and continue its efforts to end AIDS, tuberculosis (TB), and malaria worldwide.
“For 20 years, the Global Fund has been one of the most important investments the world has made in global health,” noted Bill Gates, co-chair of the Bill and Melinda Gates Foundation. “Through this record-setting replenishment, the Global Fund and its partners will save millions of lives and build sustainable health systems that can prevent future pandemics.”

Guidelines for HIV Treatment
New Updates to the Guidance for ART in Adults and Adolescents
The HHS expert panel responsible for the Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV recently updated the Guidelines to include recent scientific findings and recommendations on the following:
- antiretroviral therapy (ART) for people who become infected with HIV after having received long-acting cabotegravir for HIV PrEP;
- laboratory testing to be completed when ART begins, CD4 and viral load monitoring thereafter, and criteria for conducting drug-resistance testing when virologic failure occurs;
- optimizing ART in persons who have achieved viral suppression;
- adherence to the HIV continuum of care; and
- minor updates to Guideline sections focusing on baseline evaluation of people entering HIV care, hepatitis B/HIV coinfection, hepatitis C/HIV coinfection, and cost considerations and ART.
%20(Adobe%20stock%20images)%20small.jpeg)
Educational Resources
AIDSVu: New Blog Posts and Infographics on HIV Among Gay and Bisexual Men
In the run-up to National Gay Men’s HIV/AIDS Awareness Day (NGMHAAD) on September 27, the AIDSVu website posted several resources highlighting the impacts of HIV on gay and bisexual men. These include blog posts from Dr. Jeb Jones on HIV prevention in the internet age, particularly among gay men, and from Dr. Sean Young on digital behavior and HIV. In another blog post commemorating NGMHAAD, AIDSVu discusses the disproportional impact of HIV among gay and bisexual men, as well as racial/ethnic disparities in HIV diagnoses and on the continuum of care among gay and bisexual men. AIDSVu has also created a new set of infographics about HIV among gay and bisexual men in the U.S. These include:
- New HIV Diagnoses Among Gay and Bisexual Men: 2008-2020
- High HIV Prevalence Among Gay and Bisexual Men Over Age 55
- HIV Diagnoses by Region Among Gay and Bisexual Men in 2020
- Gay and Bisexual Men Account for More Than Half of All People with HIV
- Percentage of New HIV Diagnoses Among All Men and Among Gay and Bisexual Men in 2020
- HIV Care Continuum Among Gay and Bisexual Men by Race/Ethnicity in 2020
- Viral Suppression Rates Among Gay and Bisexual Men by Race/Ethnicity in 2020
- States with the Highest PrEP-to-MSM Ratio in 2020
- Wide Regional Variation in PrEP Use Among Gay and Bisexual Men
In Case You Missed It: Updated RWHAP Client Fact Sheets from HRSA
This summer, HRSA updated its series of one-page population fact sheets summarizing data on the approximately 562,000 clients enrolled in the Ryan White HIV/AIDS Program (RWHAP) during 2020. These resources include an overview of all RWHAP clients, together with summaries of client data for each of the selected population groups listed below. Each fact sheet generally includes information about the percentage of all RWHAP clients in the particular population group, as well as data on poverty levels, housing status, age distribution, and rates of viral suppression. Updated fact sheets are now available for the following population groups: