Inside This Issue: Updated HIV continuum of care data; status neutral HIV care; new Global Fund report; monkeypox, HIV, and STIs; viral hepatitis surveillance report; and more.
U.S. HIV/AIDS Epidemic
HIV Surveillance Report Updates Progress Toward U.S. Prevention and Care Goals
In a recent surveillance report, CDC summarizes 2020 data for Selected National HIV Prevention and Care Outcomes – indicators used to monitor progress toward U.S. national goals outlined in Healthy People 2030, the National HIV/AIDS Strategy, and the Ending the HIV Epidemic in the U.S. initiative. The report includes the latest available information on many indicators, including: the stage of HIV disease at the time of diagnosis; rates of linkage to HIV care within one month of diagnosis; receipt of HIV care and viral suppression; survival of more than 3 years after diagnosis; prescriptions, indications, and coverage for HIV pre-exposure prophylaxis (PrEP); and perinatally acquired HIV infection.
The report and associated tables include breakdowns by race/ethnicity, age, gender, transmission category, and area of residence for many of the indicators, with numerous charts, graphs, and infographics summarizing key data. Six Special Focus Profiles focus on: gay, bisexual, and other men who have sex with men; persons who inject drugs; transgender and additional gender identity persons; women (based on sex assigned at birth); persons with perinatally acquired infections; and young persons aged 13 to 24 years old.
“Data for the year 2020 should be interpreted with caution due to the impact of the COVID-19 pandemic on access to HIV testing, care-related services, and case surveillance activities in state and local jurisdiction,” according to CDC. The agency notes that the steep reduction (17%) in total U.S. HIV diagnoses during 2020 “is likely due to disruptions in clinical care services, patient hesitancy in accessing clinical services, and shortages in HIV testing reagents/materials.”
HIV Care Continuum
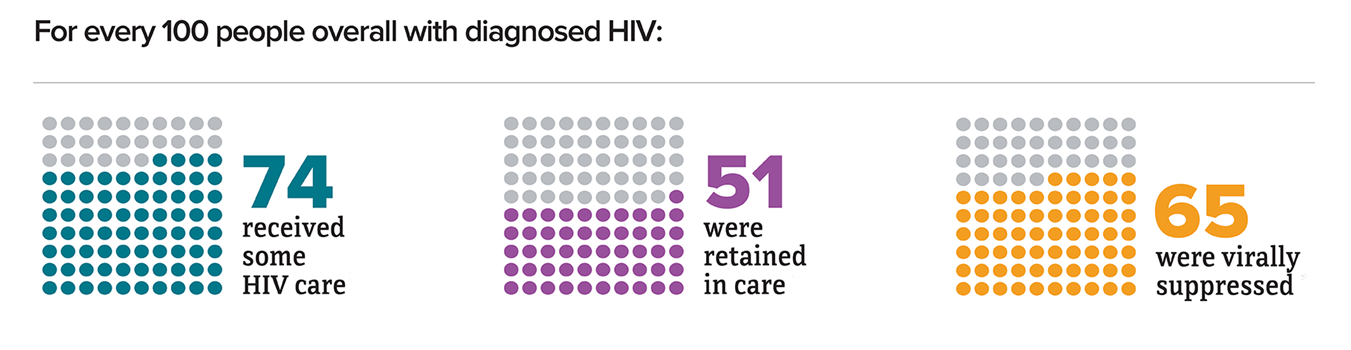
For your convenience, we have compiled and highlighted data on the HIV care continuum below, with breakdowns by race/ethnicity. These data are for the 45 states and District of Columbia with complete reporting of laboratory data to CDC. In this summary, “linkage to care” is defined as receiving at least one CD4 or viral load test within one month of diagnosis; “received some HIV care” is defined as having received at least one subsequent CD4 or viral load test; “retained in care” is defined as having had two viral load or CD4 tests at least three months apart in a year; and “viral suppression” is defined as having an HIV viral load below 200 copies/mL within 6 months of diagnosis.
- Overall: 82% linkage to care; 74% received some HIV care; 51% were retained in care; and 65% had viral suppression.
- American Indian/Alaska Native people: 80% linkage to care; 74% received some HIV care; 48% were retained in care; and 62% had viral suppression.
- Asian American people: 88% linkage to care; 73% received some HIV care; 50% were retained in care; and 68% had viral suppression.
- Black/African American people: 80% linkage to care; 72% received some HIV care; 49% were retained in care; and 60% had viral suppression.
- Hispanic/Latino people: 85% linkage to care; 71% received some HIV care; 51% were retained in care; and 63% had viral suppression.
- Native Hawaiian/Pacific Islander people: 86% linkage to care; 71% received some HIV care; 47% were retained in care; and 65% had viral suppression.
- White people: 84% linkage to care; 78% received some HIV care; 52% were retained in care; and 70% had viral suppression.
- Multiracial people: 84% linkage to care; 84% received some HIV care; 58% were retained in care; and 72% had viral suppression.
Issue Brief Outlines Benefits of Status Neutral HIV Care and Service Delivery
A status neutral framework to HIV prevention and treatment “provides care for the whole person by offering a ‘one-door’ approach: people with HIV and people seeking HIV prevention services can access treatment, prevention, and other critical services in the same place,” according to a recent CDC issue brief. This approach has the added benefits of normalizing HIV treatment and prevention and destigmatizing both. In status neutral HIV prevention and care, people whose HIV tests are negative are offered prevention tools like PrEP, condoms, harm reduction, and supportive services to stay HIV-negative. People who test HIV-positive enter primary care and are offered effective treatment and support services to help them achieve and maintain viral suppression.
This approach “can help people maintain their best health possible, while also improving outcomes in HIV prevention, diagnosis, care, and treatment,” according to CDC. “A status neutral approach to HIV-related service delivery aims to deliver high-quality, culturally affirming health care and services at every engagement, supporting optimal health for people with and without HIV.”
The CDC issue brief describes the features of status neutral HIV care and service delivery in detail, and explains how this approach can address the many barriers that can keep people from becoming engaged in HIV care, including stigma, bias, and difficulties accessing and navigating HIV care and essential support services. Short summaries are provided of several jurisdictions’ efforts to integrate a status neutral approach into their HIV care services in Chicago, New York City, Puerto Rico, Texas, and Washington, D.C. These jurisdictions have experienced important benefits from this approach, including: decreasing new HIV infections; supporting and enabling optimal health through continual engagement in comprehensive, “whole person” care; creating opportunities for more efficient service delivery; and improving health equity.
The issue brief ends with a discussion of steps CDC is taking to advance status neutral HIV care in the U.S., as well as recommended actions federal agencies, state and local health departments, healthcare providers, and community-based organizations can take to promote and integrate a status neutral approach into their programs and service delivery models.

Global HIV/AIDS Response
Global Fund Report: HIV and TB Services Rebounded in 2021
The COVID-19 pandemic had a major impact on HIV and tuberculosis (TB) services during 2020, with substantial decreases in services for HIV testing, prevention of mother-to-child transmission, male circumcision, and the initiation of treatment for HIV and TB treatment compared to 2019. Despite the continuation of the COVID-19 pandemic, these services rebounded during 2021, according to the newly released Results Report 2022 of The Global Fund to Fight AIDS, Tuberculosis, and Malaria (Global Fund). “Although most countries that fight HIV, TB and malaria have started to recover from the ravages of COVID-19, we need to accelerate our efforts if we are to fully recover lost ground and get back on track towards ending these diseases by 2030,” noted Peter Sands, executive director of the Global Fund. “By working together, the Global Fund partnership has saved 50 million lives over the past two decades, proof that global commitment and community leadership can force the world’s deadliest infectious diseases into retreat.”
Countries where the Global Fund invests achieved the following results during 2021:
- 3 million people received lifesaving antiretroviral therapy for HIV, continuing the trend of a rising number of people on treatment for the virus;
- 283,000 HIV-positive TB patients were put on antiretroviral drugs; globally, TB is the leading cause of death among people living with HIV;
- 69% of people living with HIV had a suppressed viral load;
- 5 million people were reached with HIV prevention services, including 5.8 million people from populations most at risk and 6.1 million young people – recovering the ground lost in 2020 when prevention services had declined.
- 3 million people treated for TB, including 110,000 people treated for drug-resistant TB;
- 395,000 people in contact with TB patients provided with preventive therapy;
- 280 million suspected cases of malaria were tested, and 148 million cases of malaria were treated; and
- 133 million mosquito nets were distributed to protect families from malaria.

Monkeypox Outbreak
CDC: High Rates of HIV and STIs Seen in U.S. Monkeypox Cases
The 2022 global monkeypox outbreak has affected primarily gay, bisexual, and other men who have sex with men (MSM). In addition, persons with HIV and sexually transmitted infections (STIs) are disproportionally affected by monkeypox. To increase understanding of the epidemiology and interrelationships among monkeypox, HIV, and sexually transmitted infections, CDC researchers collaborated with public health officials from eight U.S. jurisdictions to analyze data on 1,969 cases of monkeypox diagnosed between May 17 and July 22.
The researchers examined HIV and STI diagnoses among persons with monkeypox and compared differences in monkeypox clinical features according to HIV infection status. They found that the HIV prevalence rate among persons with monkeypox was 38%, and 41% had received a diagnosis of one or more other reportable STIs in the preceding year. The researchers noted that the 38% prevalence of HIV among persons with monkeypox in this study is substantially higher than the estimated national HIV prevalence among MSM (23%).
Among persons with monkeypox and diagnosed HIV infection, 94% had received HIV care in the preceding year, and 82% had a suppressed viral load. Despite their relatively high rates of HIV care and viral suppression, persons with HIV and monkeypox infection had substantially higher hospitalization rates for monkeypox than persons with monkeypox alone (8% versus 3%). Persons coinfected with HIV and monkeypox also had higher rates of several medical symptoms and conditions, including rectal pain (34% versus 26%), tenesmus (20% versus 12%), rectal bleeding (19% versus 12%), purulent or bloody stools (15% versus 8%), and proctitis (13% versus 7%).
“Increasing HIV prevalence among persons with monkeypox over time suggests that monkeypox might be increasingly transmitted among networks of persons with HIV infection, underscoring the importance of leveraging HIV and STI care and prevention delivery systems for monkeypox vaccination and prevention efforts,” the researchers noted. “Consideration should be given to prioritizing persons with HIV infection and STIs for vaccination and other prevention efforts. HIV and STI screening and other recommended preventive care should be routinely offered to persons evaluated for monkeypox, with linkage to HIV care or HIV PrEP, as appropriate.”
Steps Gay and Bisexual Men Have Taken to Prevent Monkeypox Transmission
In a separate report, CDC researchers and their colleagues summarized the findings of an online survey of 824 gay, bisexual, and other MSM during August to determine what steps, if any, they were taking to prevent transmission of the monkeypox virus. Overall, nearly half (48%) of the survey respondents reported reducing their number of sex partners, 50% reported reducing one-time sexual encounters, and 50% reported reducing sex with partners met on dating apps or at sex venues since learning about the monkeypox outbreak.
Nearly one in five respondents (19%) reported receiving at least one dose of vaccine to prevent monkeypox. Vaccination rates for monkeypox were highest among Hispanic/Latino men (27%) and lowest among non-Hispanic Black/African American men (11%), compared with 19% among non-Hispanic White men and 24% among men of other race/ethnicity.
Monkeypox vaccination rates varied widely by area of residence: 28% in urban areas, 14% in suburban areas, and 6% to 7% in less populous areas. Monkeypox vaccination rates in urban areas were much higher in urban (28%) and suburban (14%) areas than in other less populated areas (6% to 7%). Among the HIV-negative men surveyed, a much higher proportion of persons taking HIV PrEP were vaccinated (31%) than those not taking PrEP (7%) vaccinated.
“These data highlight the importance of health communication in the context of strong community leadership in response to the U.S. monkeypox outbreak,” the researchers noted. “The adoption of prevention strategies reported here aligns with specific harm reduction strategies developed for monkeypox and with broader sexual health information and recommendations for MSM.”

Viral Hepatitis
Two New CDC Reports Examine Viral Hepatitis Trends and Response
Earlier this month, CDC published Viral Hepatitis Surveillance Report – United States, 2020, which includes data on new diagnoses and mortality data related to hepatitis A (HAV), hepatitis B (HBV), and hepatitis C virus (HCV), as well as outcome data from CDC’s Perinatal Hepatitis B Prevention Program. CDC also released the 2022 Viral Hepatitis National Progress Report, which provides an update on progress toward achieving established goals for the prevention of viral hepatitis transmission, disease, and associated mortality.
During 2020, the COVID-19 pandemic caused major disruptions in access to medical care, testing, and other hepatitis-related public health activities. As a result, CDC advises that the 2020 data included in this surveillance report should be interpreted with caution. Selected highlights of the surveillance report are summarized below:
HAV: A total of 9,952 new cases of HAV were reported in the U.S. during 2020. Since CDC estimates that only about half of all HAV cases are reported, this corresponds to an estimated total of about 19,990 new HAV cases last year. HAV cases declined by nearly half (47%) from 2019 to 2020, which CDC believes may be the result of resolving outbreaks in several states during 2020. However, the estimated number of infections during that year was still about five times higher than the national goal for 2025 – which calls for reducing estimated HAV infections to 4,000.
HBV: A total of 2,157 new cases of acute HBV were reported during 2020, which corresponds to an estimated 14,000 acute HBV infections. There were also 11,635 newly reported cases of chronic HBV in 2020, which corresponds to a rate of about 5 per 100,000 population. CDC notes that, after a decade of relatively stable rates, the number of acute HBV infections decreased 32% between 2019 and 2020, probably the result of fewer people seeking healthcare and being tested for HBV during the pandemic.
HCV: Although only 4,798 new cases of acute HCV were reported during 2020, CDC estimates that the actual number of new HCV cases was about 66,700. “Since 2013, increases in injection drug use related to the nation’s drug crisis have contributed to annual increases in newly reported cases of HCV,” according to CDC. “During 2020, there was a 15% increase in the rate of reported cases of acute HCV from 2019. Although the COVID-19 pandemic disrupted health care access and reduced the number of persons tested for HCV infection, the anticipated reduction in reported cases was offset by a change to the acute hepatitis C case definition introduced in 2020.”
%202%20-%20small.jpeg)
HIV Guidelines
Recent Updates to Opportunistic Infection Guidelines for Adults, Adolescents, and Children
On September 7, HHS expert panels updated both the Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV (adult and adolescent OI guidelines) and the Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Exposed and HIV-Infected Children. The adult and adolescent OI guidelines now include updated recommendations on vaccinating persons with HIV to prevent HBV infection, invasive pneumococcal disease, and herpes zoster, as well as the use of antiretroviral treatment in persons who are hepatitis B surface antigen (HbsAg) positive. The revised OI guidelines for children include brief information about monkeypox as an OI in children, as well as the panel’s intention to include guidance on the prevention and treatment of monkeypox in children as relevant data emerge.

Educational Resources
New AIDSVu Infographics Focus on HIV Among Older Persons
AIDSVu recently published a blog item summarizing recent statistics on HIV among people aged 55 years or older in the U.S., as well as the following infographics, updated with 2020 data, focusing on this age group:
- Number of People with HIV Who Were Age 55 or Older in 2020
- New HIV Diagnoses and Deaths Among Black Americans Age 55 and Older
- New HIV Diagnoses Among Women Are Concentrated in Older Age Groups
- Increase in HIV PrEP Use Among Persons Age 55 or Older
- PrEP-to-Need Ratio Among Persons Age 55 or Older
- HIV Care Continuum Among Persons Age 55 or Older
- Social Determinants of Health Among Older People with HIV