Inside This Issue: Overview of U.S. HIV epidemic; HHS declares Monkeypox a Public Health Emergency; FDA authorizes emergency use of JYNNEOS vaccine; streamlined COVID-19 guidance from CDC; rapid rise in U.S. overdose death rates; and more.
HIV Care and Treatment
Latest MMP Report Provides Detailed Overview of U.S. HIV Epidemic in 2020
The U.S. Centers for Disease Control and Prevention (CDC) recently published the latest update in its Behavioral and Clinical Characteristics of Persons with Diagnosed HIV Infection Medical Monitoring Project (MMP) report series, which provides extensive information about the state of the U.S. HIV epidemic during 2020. The report summarizes data from the MMP, a cross-sectional, nationally representative sample survey that assesses the behavioral and clinical characteristics of adults with diagnosed HIV infection in the United States. The MMP also provides information on behaviors and clinical outcomes that affect the risk of HIV transmission, morbidity, and mortality that are critical for achieving the goals of the National HIV/AIDS Strategy and the Ending the HIV Epidemic in the U.S. initiative.
Many of the key findings of the report are summarized in a series of infographics, including the following:
HIV medical care and treatment among people with diagnosed HIV: The MMP data indicated that 80% of people diagnosed with HIV did not miss any HIV medical care appointments during the previous 12 months; 95% were currently taking antiretroviral therapy (ART), and 62% took all their prescribed ART doses during the previous 30 days.
Barriers to HIV treatment among people with diagnosed HIV: The top reasons people reported for not taking ART were money or insurance problems (37%), never discussing restarting ART with their healthcare provider (29%), and concerns that taking ART would make them sick or harm them (20%).
People’s top reasons for missing at least one ART dose during the previous 30 days were forgetting (65%), change in daily routine or being away from home (39%), and falling asleep or oversleeping (37%).
Socioeconomic status, behaviors, and medical issues among people with diagnosed HIV: nearly 1 in 10 experienced homelessness; 1 in 6 experienced food insecurity; nearly 4 in 10 households lived at or below the poverty threshold; 1 in 6 engaged in binge drinking; 1 in 3 used drugs for nonmedical purposes; 4 in 10 had a disability; and 1 in 5 had symptoms of depression or anxiety.
Median HIV stigma score: An important goal of U.S. HIV response strategies is to eliminate HIV stigma. On a scale of 0 (no stigma) to 100 (high stigma), the median score for persons with HIV was 28.
Need for HIV ancillary services: 41% of people with HIV reported needing, but not receiving, one or more ancillary services in the previous 12 months. The most common ancillary services needed but not received were dental care (21%), SNAP/WIC nutrition assistance (10%), and shelter/housing (8%).
Ryan White HIV/AIDS Program (RWHAP) coverage: 47% of people with diagnosed HIV had RWHAP coverage.
Sexual behaviors among people with diagnosed HIV: 13% of cisgender men who have sex with cisgender men, 13% of cisgender men who have sex with cisgender women, and 14% of cisgender women who have sex with cisgender men reported having sex without using any HIV prevention strategy during the previous year.
The full report has an extensive commentary on its findings and a series of tables and figures that provide data breakdowns by gender, sexual orientation, race/ethnicity, age, education levels, country or territory of birth, housing status, incarceration history, food insecurity, household income and poverty status, health insurance and disability coverage, self-assessment of general health, and years since HIV diagnosis.
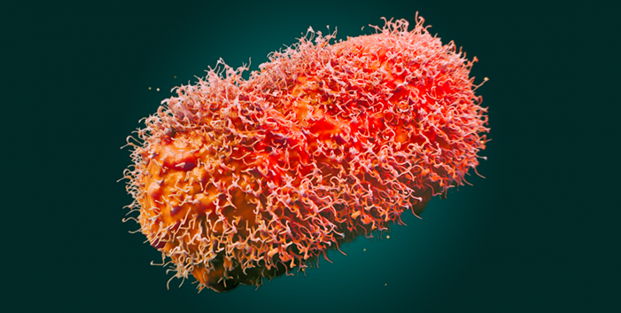
Monkeypox Outbreak and Response
HHS Declares Monkeypox a Public Health Emergency
On August 4, Department of Health and Human Services (HHS) Secretary Xavier Becerra declared the ongoing spread of monkeypox virus in the U.S. to be a public health emergency. “Ending the monkeypox outbreak is a critical priority for the Biden-Harris Administration. We are taking our response to the next level by declaring a public health emergency,” said Secretary Becerra. “With today’s declaration we can further strengthen and accelerate our response.”
HHS noted that the declaration of a public health emergency for monkeypox is in concert with Food and Drug Administration’s (FDA) work to increase the availability of monkeypox vaccines across the country, including using a new dose-sparing approach that could increase the number of doses available up to five-fold. (For more information, see the next article in this newsletter.)
The public health emergency also carries important implications for data sharing with the federal government. At the time the declaration was issued, 51 jurisdictions had already signed data use agreements that will provide CDC with information related to vaccine administration. Declaring the outbreak an emergency may encourage additional jurisdictions to share data with CDC. The declaration also authorizes the Centers for Medicare & Medicaid Services to collect testing and hospitalization data.
FDA Authorizes Emergency Use of JYNNEOS Vaccine to Increase Vaccine Supply for Monkeypox
On August 9, the FDA issued an emergency use authorization (EUA) that allows healthcare providers to administer the JYNNEOS vaccine by intradermal injection to persons aged 18 years or older who are at high risk for monkeypox infection. The EUA also allows the JYNNEOS vaccine to be administered by subcutaneous injection in persons younger than 18 who are at high risk of monkeypox infection.
The JYNNEOS vaccine was approved in 2019 for prevention of smallpox and monkeypox disease in adults aged 18 years or older determined to be at high risk for smallpox or monkeypox infection. JYNNEOS has been administered subcutaneously as two doses, four weeks apart. However, the recent EUA now allows a fraction of the vaccine dose to be administered intradermally for persons aged 18 years or older. Two doses of the vaccine given four weeks apart will still be needed. FDA expects that the EUA will increase the total number of doses available for use by up to five-fold.
“In recent weeks the monkeypox virus has continued to spread at a rate that has made it clear our current vaccine supply will not meet the current demand,” noted FDA Commissioner Dr. Robert Califf. “The FDA quickly explored other scientifically appropriate options to facilitate access to the vaccine for all impacted individuals. By increasing the number of available doses, more individuals who want to be vaccinated against monkeypox will now have the opportunity to do so.”
The agency also recently launched the FDA Monkeypox Response website, which includes information about FDA’s role in responding to the outbreak and public emergency, a “fast facts” question-and-answer section about monkeypox, as well as information about monkeypox vaccines, therapeutics, diagnostics, fraud and misinformation, and additional resources.
CDC Issues Guidance on the Prevention and Treatment of Monkeypox in Persons with HIV
As part of its ongoing response to the multinational outbreak of monkeypox in recent months, CDC issued Interim Guidance for Prevention and Treatment of Monkeypox in Persons with HIV on August 5. The outbreak, which is centered in the U.S. and Europe, has disproportionately affected gay, bisexual, and other men who have sex with men, including persons with HIV.
The interim guidance includes the following recommendations:
- “Providers should consider both viral suppression and CD4 count in weighing the risk for severe monkeypox-associated outcomes for any patient with HIV infection. Although severe outcomes have been observed in persons with inadequately treated HIV infection who have CD4 counts ≤350 per μL and are likely not virologically suppressed, currently available data are insufficient to define actionable thresholds.”
- “When vaccination is used for prevention of monkeypox in persons with HIV infection, JYNNEOS is preferred over ACAM2000. Based on current recommendations from ACIP [CDC's Advisory Committee on Immunization Practices], ACAM2000 is contraindicated for persons with HIV infection because of the risk for severe adverse effects resulting from the spread of vaccinia virus. If high-risk exposures cannot be avoided, immunocompromised persons may receive JYNNEOS in consultation with their health care provider after careful consideration of the risks and benefits.”
- “Persons with and without HIV infection should follow the same guidance to protect themselves from monkeypox. Primary prevention of monkeypox includes isolating persons with infection from other persons and their pets, avoiding close contact and sexual activity (including oral, anal, and vaginal sex or sharing of sex toys) with persons with infection, and postexposure vaccination. Persons identified as close contacts of persons with monkeypox should follow any additional guidance from their state or local health department.”
In related news, the expert panel responsible for updating Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV recently modified the guidelines to include information about monkeypox and a link to CDC’s guidance above, as well as a commitment to add information about monkeypox as an HIV-related opportunistic infection as relevant data emerge.
In addition, Dr. Laura Cheever, the associate administrator of HRSA’s HIV/AIDS Bureau has written a “Dear Colleagues” letter to Ryan White HIV/AIDS Program (RWHAP) recipients providing an update on the U.S. monkeypox outbreak, as well as information on vaccination, testing, treatment, and the availability of RWHAP funds to provide monkeypox-related treatment and medical services to eligible clients.
The COVID-19 Pandemic
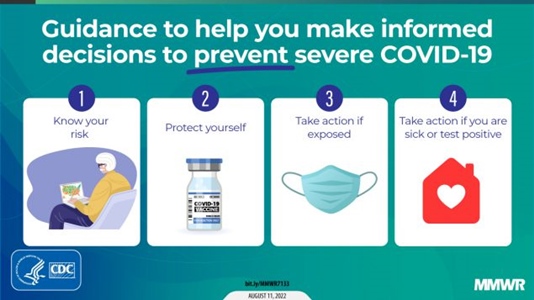
Streamlined COVID-19 Guidance from CDC
Earlier this month, CDC issued revised guidance to minimize the impact of COVID-19 on individuals, communities, and healthcare systems. The updated guidance is designed “to help people better understand their risk, how to protect themselves and others, what actions to take if exposed to COVID-19, and what actions to take if they are sick or test positive for the virus,” according to CDC.
“We’re in a stronger place today as a nation, with more tools – like vaccination, boosters, and treatments – to protect ourselves, and our communities, from severe illness from COVID-19,” noted Dr. Greta Massetti of CDC’s COVID-19 Emergency Response Team. “We also have a better understanding of how to protect people from being exposed to the virus, like wearing high-quality masks, testing, and improved ventilation. This guidance acknowledges that the pandemic is not over, but also helps us move to a point where COVID-19 no longer severely disrupts our daily lives.”
In its streamlined guidance, CDC is:
- continuing to promote the importance of being up to date with vaccination to protect people against serious illness, hospitalization, and death;
- updating its recommendations for people who are not up to date on COVID-19 vaccines on what to do if exposed to someone with COVID-19;
- recommending that, instead of quarantining, people exposed to COVID-19 wear a high-quality mask for 10 days and get tested on day 5;
- reiterating that, regardless of vaccination status, people should isolate from others if they have COVID-19;
- recommending that people should also isolate themselves from others if they are sick and suspect they have COVID-19 but have not yet received test results;
- recommending that people with positive COVID-19 test results follow CDC’s full isolation recommendations, while those who test negative can end their isolation;
- recommending that people who test positive for COVID-19 stay home for at least 5 days, isolate themselves from others in their home, and wear a high-quality mask when they must be around others at home and in public.
- advising that people with COVID-19 may end their isolation after day 6 if they are fever-free for 24 hours without the use of medication, and their symptoms are improving, or they never had symptoms;
- advising people with COVID-19 to avoid being around people who are more likely to get very sick from COVID-19 until at least day 11;
- advising people with HIV to continue wearing a high-quality mask through day 10;
- recommending that people who had moderate or severe illness due to COVID-19 or who have a weakened immune system continue to isolate through day 10;
- recommending that people who have severe illness or have a weakened immune system consult their doctor before ending isolation; and
- clarifying that people who have ended isolation should restart their isolation at day 0 if their COVID-19 symptoms worsen, and should talk to a healthcare provider.
In addition, in most community settings, CDC is no longer recommending COVID-19 screening testing of asymptomatic people without known exposures.

The U.S. Opioid Epidemic
Rapid Rise in Drug Overdose Death Rates, Particularly Among Black Persons and American Indian and Alaska Native Persons
During 2020, nearly 92,000 drug overdose deaths occurred in the U.S. – with an age-adjusted rate of 28.3 per 100,000 population. This 2020 death rate was 31% higher than the rate of 21.6 per 100,000 in 2019. Opioids accounted for three-quarters (74.8%) of the overdose deaths during 2020, and more than 80% of opioid deaths involved synthetic opioids.
To learn more about patterns and disparities in overdose death rates, CDC researchers and their colleagues recently analyzed data from the State Unintentional Drug Overdose Reporting System (SUDORS) in the 25 states and the District of Columbia that submitted complete overdose data. They examined patterns in death rates by race and ethnicity and county-level social determinants of health (such as income inequality and treatment provider availability).
The analysis revealed substantial disparities in the rise in overdose death rates by race/ethnicity, gender, and age. Although overdose death rates increased in nearly all racial and ethnic groups, the rise among non-Hispanic Black (Black) and American Indian or Alaska Native (AI/AN) persons, – 44% and 39%, respectively – was far greater than that among Whites (22%).
Among demographic subgroups, the overdose death rate for Black males age 65 years or older increased to nearly seven times that of White males of the same age during 2020. In addition, the death rate among AI/AN females between 25 and 44 years old rose to nearly twice that of White females of the same age. The analysis also showed that drug overdose death rates, particularly among Black persons, were higher in counties with greater levels of income inequality. For Black persons, the death rates in the counties with the greatest income inequality were more than twice as high as those in counties with the least income inequality.
The researchers concluded that, “Implementation of available, evidence-based, culturally responsive overdose prevention and response efforts that address health disparities impacting disproportionately affected populations are urgently needed.”
Viral Hepatitis
NIH Updates Strategic Plan to Cure Hepatitis B
As part of its ongoing effort to increase the scientific understanding of hepatitis B virus (HBV), discover a cure, and end the HBV epidemic, the National Institutes of Health (NIH) recently updated the Strategic Plan for NIH Research to Cure Hepatitis B. “The revised plan incorporates lessons from the COVID-19 pandemic and recent advances in technology,” according to NIH. “The plan aligns with the Department of Health and Human Services’ Viral Hepatitis National Strategic Plan and is designed to be a part of the agency’s ongoing response to the effects of this disease.”
NIH’s updated HBV strategic plan highlights three key research priorities:
- Improving the understanding of HBV biology, including how the virus is transmitted and causes disease. This is expected to contribute to the development of the next-generation therapeutics and vaccines needed to cure HBV and control the virus.
- Developing tools and resources to fight HBV, including new cell culture systems, cell-free systems, and animal models to advance hepatitis research. “Identifying better biomarkers and developing improved diagnostics would allow researchers to track disease progression in people with hepatitis B and enhance clinical research,” according to NIH.
- Creating strategies to cure and prevent HBV, including efforts to develop and test promising HBV therapeutics and vaccines. “Using strategies learned from the COVID-19 pandemic to reach and evaluate treatments in at-risk populations, including racial and ethnic minority groups, NIH can conduct clinical trials that are relevant to individuals most in need of a HBV cure.”
.png)
Reports and Educational Resources
AIDSVu Data Shows Substantial Inequities in PrEP Use by Race/Ethnicity and Region
At the recently concluded International AIDS Conference, AIDSVu released the first publicly available state-level data on the use of HIV pre-exposure prophylaxis (PrEP) by race/ethnicity for the period 2012 to 2021. The data indicate that, while PrEP use rose an average of 56% each year since its approval in 2012, there remain significant inequities in PrEP use among Black and Hispanic people and in the U.S. South. According to AIDSVu, there were only 3 Black and 6 Hispanic/Latinx PrEP users for each new HIV diagnosis within those racial/ethnic groups, compared to 26 White PrEP users for each new HIV diagnosis among White people. There were also significant inequities in PrEP use by region. Overall, in the U.S. South, there were only 7 PrEP users for each new HIV diagnosis, compared to 15 PrEP users for each new HIV diagnosis in the Northeast.
“HIV prevention programs should be guided by PrEP use equity – the use of PrEP relative to the impact of the HIV epidemic on that group. Today’s data shows that we have a long way to go,” noted Dr. Patrick Sullivan, principal scientist for AIDSVu. “It is important that data do not live in a vacuum and that the insights we glean from research are translated into policy and action.”
He said that drawing attention to communities and geographic regions underserved by PrEP may help prevention programs better allocate resources to ensure that PrEP reaches those with the greatest unmet need. In addition to its summary of the new PrEP data analysis, AIDSVu published two blog items discussing the significance of its findings and reviewing the past, present, and future of PrEP.
Recent HIV Reports from CDC
In addition to its report on the behavioral and clinical characteristics of persons with HIV (summarized in the first article of this issue), CDC recently issued two other reports focusing on HIV surveillance and program evaluation.
The latest report in the series of Core Indicators for Monitoring the Ending the HIV Epidemic in the United States Initiative presents data reported to CDC on HIV diagnoses for the period from January 2021 through March 2022; prompt linkage to HIV care after diagnosis during 2021; and PrEP prescriptions and coverage from January 2019 through December 2021. Associated data tables include breakdowns by gender, age at diagnosis, race/ethnicity, transmission category (for diagnoses and linkage to care only), and region of residence.
Integrated HIV Surveillance & Prevention Programs for Health Departments (PS18-1802): Monitoring and Evaluation Report, 2020 – This report provides an overview of select PS18-1802 Component A prevention program components in 60 CDC-funded health departments in the U.S., Puerto Rico, and the U.S. Virgin Islands during 2020. In particular, the report summarizes program accomplishments in HIV testing, program integration, linkage to HIV medical care, partner services, HIV prevention services, and PrEP awareness, use, and support.
.jpg)
Other COVID-19 News
Important Update to Treatment Guidelines for COVID-19
The NIH also issued a major update to its Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. The updated guidelines include a new section, “Special Considerations in People Who Are Immunocompromised.” This patient group includes people with advanced or untreated HIV infection, defined as a CD4 T lymphocyte cell counts under 200 cells/mm3, a history of an AIDS-defining illness without immune reconstitution, or clinical manifestations of symptomatic HIV.
“This section covers methods of preventing SARS-CoV-2 infection, including vaccinating patients and their close contacts against COVID-19 and using tixagevimab plus cilgavimab (Evusheld) as pre-exposure prophylaxis,” according to NIH. “It also discusses considerations for clinicians who manage patients with COVID-19 who are immunocompromised. Key considerations include consulting with specialists before stopping or reducing doses of immunosuppressive drugs, promptly initiating antiviral drugs or anti-SARS-CoV-2 monoclonal antibodies in patients with mild to moderate disease, managing concomitant medications and drug-drug interactions, and monitoring for secondary infections.”
COVID-19 Summaries and Research Reports
CDC’s COVID Data Tracker Weekly Review highlights key data from its COVID Data Tracker, narrative interpretations of the data, and visualizations from the week. Themes of recent Weekly Review issues include returning to school; COVID-19 vaccine equity; protecting healthcare providers and public health workers; rising cases due to the Omicron BA.5 variant; and COVID-19 vaccination and booster recommendations.
The Morbidity and Mortality Weekly Report (MMWR) is also providing continuing coverage of COVID-19-related research. CDC is archiving its MMWR reports on a page devoted to studies about COVID-19. For your convenience, we have compiled below links to recent MMWR papers:
Vaccination
COVID-19 in Children and Adolescents
Other Topics




.png)
