Inside This Issue: HIV and social determinants of health, rising opioid death rates, collaborative efforts to cure HIV and sickle cell disease, HIV prevention and treatment toolkits, HIV services in prisons.
HIV and Social Determinants of Health
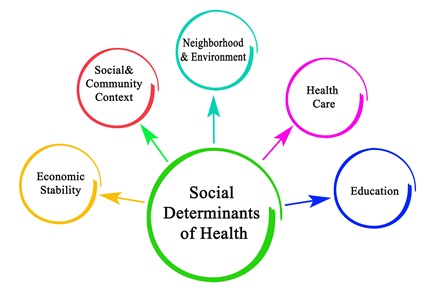
CDC Report Examines Social Determinants of Health Among HIV+ Adults
In 2017, new HIV diagnoses were more common in areas where: the median household incomes are low; a relatively high percentage of persons are living below the federal poverty line; a relatively high percentage of adults lack a high school education; and a relatively high percentage of persons lack health coverage. These are some of the findings of the recent CDC surveillance report, Social Determinants of Health Among Adults with Diagnosed HIV Infection, 2017. “The term social determinants of health (SDH) refers to the overlapping social structures and economic systems (e.g., social environment, physical environment, health services, and structural and societal factors) that are responsible for most health inequities,” according to CDC. “Stratifying public health data by key SDH is useful in monitoring health inequities.”
This SDH surveillance report presents data on persons aged 18 years and older with HIV infection diagnosed in 2017 and reported to the National HIV Surveillance System (NHSS) through December 2018. The report focuses on four SDH indicators:
1) federal poverty status: the proportion of residents aged 18 years and older in the U.S. census tract who were living below the U.S. poverty level at any time during the 12 months before the survey response;
2) education level: the proportion of residents aged 18 years and older in the census tract with less than a high school diploma;
3) median household income: the median income for a household within the census tract during the 12 months before the survey response; and
4) health insurance coverage: the proportion of residents aged 18 years and older in the census tract without health insurance or a health coverage plan.
The report provides breakdowns of the SDH and HIV diagnosis data by gender, race/ethnicity, age, transmission category, and area of residence. Some selected highlights by gender are presented below. Please note that all rates are per 100,000 population.
- Poverty status: The highest HIV diagnosis rates for males (40.1) and females (10.1) were among those who lived in census tracts where 19% or more of the residents lived below the federal poverty level. For both sexes, the rate of HIV diagnoses increased as the percentage of residents living below the federal poverty level increased.
- Education levels: The highest HIV diagnosis rates for males (35.1) and females (9.4) were among those who lived in census tracts where 18% or more of the residents had less than a high school diploma. For both sexes, the rate of HIV diagnoses increased as the percentage of residents with less than a high school diploma increased.
- Household income: The highest HIV diagnosis rates for males (39.3) and females (10.2) were among those who lived in census tracts where the median household income was less than $40,000 a year. For both sexes, the rate of HIV diagnoses decreased as the median household income increased.
- Health coverage: The highest HIV diagnosis rates for males (38.6) and females (9.5) were among those who lived in census tracts where 16% or more of the residents did not have health insurance or a health coverage plan. For both sexes, the rate of HIV diagnoses increased as the percentage of uninsured persons increased.
“Addressing the SDH that adversely affect health outcomes may advance efforts in reducing disparities in HIV diagnosis rates between populations,” the report notes. “Addressing SDH also helps to quantify health differences between populations or geographic areas and can provide insight for identifying populations or areas that may benefit from HIV testing, prevention, and treatment initiatives.”
%20small.jpeg)
The U.S. Opioid Epidemic
Opioid Overdose Death Rates Spike Among Urban Middle-Aged Blacks and Younger Whites
U.S. drug overdose deaths involving opioids increased six-fold between 1999 and 2017, rising from about 8,000 to nearly 48,000. The growing use of illicitly manufactured fentanyl (IMF) and fentanyl analog drugs have fueled recent rises in opioid-involved overdose deaths. In 2017 – the most recent year for which detailed data are available – synthetic opioids were involved in nearly 60% of opioid-involved overdose deaths. With the rising use of IMF, opioid-involved overdose deaths have also increased among minority population groups, including non-Hispanic Blacks (Blacks) and Hispanics – groups that have historically had relatively low opioid-involved overdose death rates. In addition, metropolitan areas have experienced sharp increases in drug and opioid-involved overdose deaths since 2013. However, until now, detailed breakdowns of overdose data by race/ethnicity and age in metropolitan areas have not been available.
To shed further light on trends in opioid-involved deaths, an HHS/CDC research team has analyzed opioid overdose death rates among persons aged 18 years or older during the period 2015 through 2017 across U.S. metropolitan areas. Their analysis shows that nearly all racial/ethnic groups and age groups experienced increases in opioid-involved and synthetic opioid–involved overdose death rates during the period. The groups with the greatest increases were:
- Blacks aged 45-54 years living in large central metro areas, with rates rising from 19.3 to 41.9 per 100,000;
- Blacks aged 55-64 years living in large central metro areas, with rates increasing from 21.8 to 42.7 per 100,000; and
- Non-Hispanic Whites aged 25-34 years living in large fringe metro areas, with rates rising from 36.9 to 58.3 per 100,000.
“The changing patterns of the opioid overdose epidemic necessitate a rapid, culturally tailored and multifaceted public health response that appropriately targets and incorporates the needs of evolving populations at risk, including minority populations that historically have been regarded as having low opioid-involved overdose death rates,” the HHS/CDC researchers note. “This study emphasizes the importance of data-informed approaches to addressing the evolving needs of communities and highlights the need for timely data that can be used to effectively guide public health responses.”
.jpg)
Cure Research
NIH Launches $200 Million+ Collaboration to Develop Gene-Based Cures for HIV and Sickle Cell Disease
The National Institutes of Health (NIH) recently announced plans to invest at least $100 million during the next four years to support the development of affordable, gene-based cures for HIV and sickle cell disease (SCD). The Bill & Melinda Gates Foundation has also agreed to invest $100 million toward this goal. Any treatments that are developed as a result of this collaborative effort will be made available worldwide, including in low-resource areas such as sub-Saharan Africa, where the prevalence of both HIV and SCD are high.
“Dramatic advances in genetics over the last decade have made effective gene-based treatments a reality, including new treatments for blindness and certain types of leukemia,” according to NIH. “Yet these breakthroughs are largely inaccessible to most of the world by virtue of the complexity and cost of treatment requirements, which currently limit their administration to hospitals in wealthy countries.”
The NIH and Gates Foundation initiative has the goal of advancing safe, effective, and durable gene-based cures to clinical trials in the U.S. and countries in sub-Saharan Africa within the next 7 to 10 years. “This unprecedented collaboration focuses from the get-go on access, scalability, and affordability of advanced gene-based strategies for sickle cell disease and HIV to make sure everybody, everywhere has the opportunity to be cured, not just those in high-income countries,” notes NIH Director Francis Collins.
.jpg)
HIV Prevention and Treatment
NIAID: Optimizing HIV Prevention and Treatment Toolkits Can Help End the Epidemic
“Unprecedented basic and clinical biomedical research advances over the past 4 decades have led to the development of ‘toolkits’ of highly effective interventions for preventing and treating HIV,” according to a recent journal commentary written by Anthony Fauci, director of the National Institute for Allergy and Infectious Diseases (NIAID), and his colleagues. Theoretically, the widespread distribution of antiretroviral therapy (ART) to people living with HIV and pre-exposure prophylaxis (PrEP) to persons at high risk for infection could end the HIV pandemic. However, major “implementation gaps” between what is theoretically possible and what is currently being achieved have prevented HIV prevention and treatment interventions from reaching their full potential.
“It is essential that we maximally implement these existing interventions while continuing to pursue the discovery and development of innovative approaches, novel technologies, and experimental interventions,” the NIAID researchers note. These include new forms of PrEP and long-acting ART regimens that might be more effective and achieve greater coverage, because they are considered more acceptable and easier to use by people living with HIV or at risk for infection. The development of an HIV vaccine could also have a major impact on the course of the epidemic in the decades ahead. One current model of the global HIV epidemic indicates that, if the status quo of HIV prevention treatment is maintained, there will be approximately 49 million new HIV cases between 2015 and 2035. However, the NIAID authors note that the availability and deployment of an HIV vaccine with just 50% efficacy could potentially avert about one-third – 17 million – of these infections.
%20small.jpg)
HIV in Prison
UNAIDS: Many Prisoners Worldwide Lack Basic HIV Services
Globally, incarcerated persons have HIV prevalence rates averaging about five times higher than the general population, according to UNAIDS. A variety of environmental, social, cultural, human rights, and biological factors contribute to this disparity. These include risk behaviors, such as sharing of used needles and syringes and unprotected sex, as well as factors including exposure to sexual violence and the lack of access to comprehensive HIV prevention and harm reduction services.
In addition, specific at-risk population groups – people who inject drugs, sex workers and, in some countries, transgender people, gay men, and other men who have sex with men – tend to be overrepresented among incarcerated populations. UNAIDS notes that, “Despite the relative ease of reaching people within prisons, HIV services are not provided in prisons in many countries.” During the period 2016 through 2018, while 83 countries reported offering HIV testing in prisons and 74 offered some antiretroviral therapy, relatively few offered other important HIV services. Only 32 countries reported providing condoms in prisons, only 24 countries reported offering opioid substitution therapy, and just 3 countries reported providing sterile injecting equipment in prisons.

Guidelines
HHS Publishes Updates to Adult and Pediatric Opportunistic Infection Guidelines
In recent weeks, the U.S. Department of Health and Human Services (HHS) has updated several sections of its adult and pediatric guidelines for the prevention and treatment of opportunistic infections, which are posted on its AIDSinfo site. The affected sections, together with links to a summary of the recent changes, are presented below:
- The Community-Acquired Pneumonia (CAP) section has been modified to include new information on the epidemiology of CAP, the strength of recommendations for managing CAP, and references supporting these changes.
- Three tables on drug interactions, side effects, and drug dosing adjustment for persons with renal insufficiency have also been changed to incorporate the latest available information.
- These changes are described in greater detail in the What’s New section of these guidelines.
- The section on Vaccine-Preventable Diseases in Children and Adolescents with HIV Infection has been updated to include information about new vaccines available for the prevention of meningococcal infection and human papillomavirus, and to include an expanded discussion of yellow fever vaccine recommendations for children with HIV.
- These changes are described in greater detail in the What’s New section of these guidelines.



